Legislative Session Starts; MMA to Focus on 5 Major Issues
February 19, 2026
State lawmakers returned to St. Paul on February 17 for the second half of the 2025-2026 biennium.
February 26, 2025
Legislation to increase Medical Assistance (MA) reimbursements for outpatient services to 100% of the Medicare level (SF 1402, Wiklund, DFL – Bloomington) passed out of the Senate Health and Human Services Committee on February 26 and was referred to the Senate Taxes Committee.
The legislation would implement the Department of Human Services (DHS) study recommendations from 2024 to increase community mental health and outpatient MA reimbursement rates to Medicare levels. The proposal includes a funding mechanism which maximizes available federal funds through an assessment on managed care organizations (MCOs).
 |
|
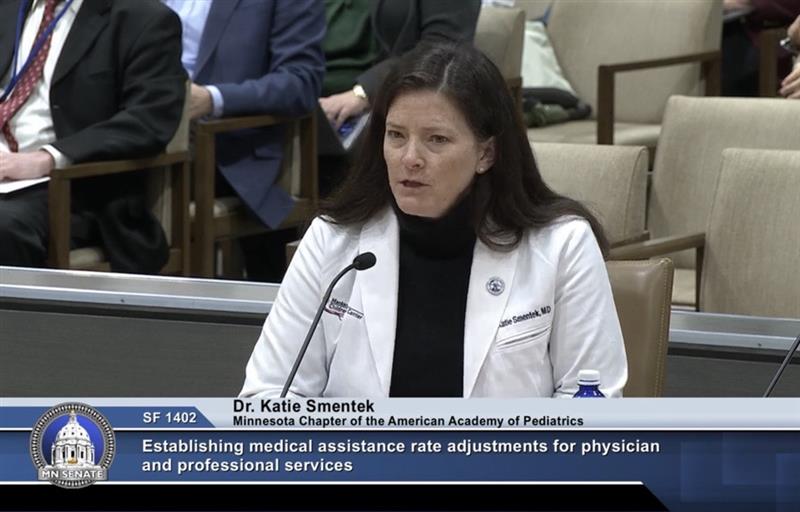
Katie Smentek, MD, testifies on behalf of the MMA and the Minnesota Chapter of the American Academy of Pediatrics. |
“I am a pediatrician from Mankato, where I’ve worked for 17 years,” said Katie Smentek, MD, on behalf of the MMA and the Minnesota Chapter of the American Academy of Pediatrics. “I see patients every day who rely on medical assistance for their healthcare. The increased reimbursement rates proposed in this bill will 1) improve access to care and 2) advance health equity for all Minnesota patients, in every corner of the state.”
The number of Minnesotans on MA has grown substantially in recent years. About one in four Minnesotans are covered by MA, and more than 40% of babies born in Minnesota are covered by MA.
Minnesota has not seen an across the board increase in MA rates in decades. Currently, MA reimburses at 60-70% of Medicare, and only about 30% of what commercial insurers pay. Minnesota’s current payment levels rank 31st in the nation. The proposed rate increase would improve that rank to sixth in the nation. MA patients live in every corner of the state, with a larger disproportionate share living in rural and traditionally underserved communities across Minnesota. The legislation ensures those most in need have access to care.
Proponents of the bill include a broad coalition of physician specialty societies, health systems, mental health advocacy organizations, patient advocacy groups, healthcare access advocacy groups, and other healthcare provider groups.
“MA reimbursement rates are extremely low compared to the cost of providing care,” said the bill’s author, Sen. Melissa Wiklund. “Because we have left our rates unchanged for so long, these increases come with a significant cost, and we are all well aware of our future budget projections. The good news is we have an opportunity to increase these rates in a fiscally responsible way relying on our health plans to partner with us to accomplish our shared goals. As amended, my bill uses a health plan assessment to leverage federal matching funds. By using a federally allowable Medicaid funding mechanism, our MCO partners get back 99% of their assessment through higher capitation rates. The assessment is determined on a per enrollee basis and applies to all health plan companies in Minnesota. There are also different tiers and assessment rates, all designed to minimize the impact on health plans.”
The Minnesota Council of Health Plans and the Minnesota Chamber of Commerce shared their concerns with the use of an MCO assessment to pay for the bill.
The House companion, HF 1005 (Bierman, DFL – Apple Valley) was referred to the Human Services Finance and Policy Committee, and is waiting to receive its first hearing.
February 19, 2026
State lawmakers returned to St. Paul on February 17 for the second half of the 2025-2026 biennium.
February 19, 2026
On the second day of the legislative session, MMA leadership was already advocating for one of its top priorities - minimizing the harm of federal changes to Medical Assistance (MA).
February 19, 2026
Legislation to prohibit the use of artificial intelligence (AI) in prior authorization requirements was heard in the House Commerce Finance and Policy Committee on February 19.